21 March 2011
This was my final week of placement as a student. It was quite daunting as I was very conscious of the fact that the next time I work in a radiography department I will be a qualified radiographer. It was also very exciting as, after 5 years, I can now see the end of the course in sight.
During the week I carried out a general practitioner (GP) request on a female patient who had presented to her GP with pain and tenderness in her forearm. The clinical history was brief so I asked the patient for more details. She showed the area of the pain which looked a little swollen but nothing remarkable. She informed me there had been no trauma and she didn’t understand why it was painful. I then continued with the examination of an AP and lateral forearm.
On processing the image it was very clear there was something obviously amiss with the patients’ ulnar. It looked as if something had taken a clean bite out of the patients’ bone, I had seen a similar case previously and thought it looked like osteosarcoma. I asked another radiographer for her opinion and we decided to get a radiologist to have a look before letting the patient leave. It was the opinion of the radiologist that the patient did have osteosarcoma and he was going to telephone her GP straight away so she could get an urgent referral to the osteosarcoma team.
I found the patients symptoms for this very surprising and I could understand why it took her so long to visit her doctor. The patient was 32 years of age with an 18 month old baby so it was understandable that she first thought she may have bumped it without realising and it would get better.
Osteosarcoma is a primary malignant tumour of bone and the cause of it is unknown. According to Shenoy at el (2007) osteosarcoma is the most common malignant bone tumour which conflicts with the opinion of Pretorius and Jeffrey (2006) who state osteosarcoma as being the second most common primary bone tumour after multiple myeloma. It is also the opinion of Pretorius and Jeffrey (2006) that sarcomas tend to undergo hematogenous spread, with pulmonary metastases being the most common.
According to Wang and Houston (2005) most osteosarcomas are sporadic, whereas inherited predisposition accounts for a small number of cases, along with this 20% of patients with osteosarcoma present clinically with overt metastatic disease, with the presence of metastatic disease being a strong predictor of a poor outcome. The disease is believed to originate from primitive mesenchymal cells but also may arise from pluripotential mesenchymal cells. Osteosarcoma is a deadly cancer and is commonly fatal when it metastasizes to the lungs. It usually forms as a single lesion on long bones, with the distal femur being the most common, then the proximal humerus and proximal tibia.
Several tests are necessary to diagnose osteosarcoma. Initially, a blood test followed by imaging tests to detect any other tumours and their location within the body. This can be performed by an X-ray, MRI, CT scan or bone scan. Confirmation of osteosarcoma can also be done by performing a biopsy to remove a piece of bone tissue.
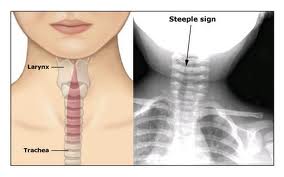
Treatment for osteosarcoma depends on the location of the tumour and the severity of the illness. Treatments may include neoadjuvant therapy which is the administration of a therapeutic agent before the main treatment of chemotherapy to destroy cancerous cells and prevent the growth of new malignant cells. The aim of neoadjuvant therapy is to reduce the size or extent of the cancer before using radical treatment intervention, thus making procedures easier, more likely to succeed, and reducing the consequences of a more extensive treatment technique that would be required if the tumour wasn’t reduced in size or extent. Additionally, radiation therapy, which uses high-energy radiation beams to shrink tumours and destroy cancer cells may also be used to treat osteosarcoma. In advanced stages of osteosarcoma, doctors may suggest amputation to remove the affected limb. Advances in surgical techniques have allowed a reduction in the number of amputations associated with osteosarcoma. Tumours can now be removed from the affected bone without removing a limb, this is done by using artificial bones or bones from other parts of the body. These advances in surgical techniques to treat osteosarcoma have resulted in higher survival rates, and high limb salvage rates associated with this type of cancer. Attached to this writing are images taken from x-ray 2000 and the childrens specialist website.
Pretorius, E. S. and Jeffrey A. S. 2006. Radiology secrets. 2nd ed. Philadelphia: Mosby Elsevier
Shenoy, R. Pillai, A. Sokhi, K. Porter, D. Ried, R. 2008. Survival trends in osteosarcoma of humerus. European Journal of Cancer Care 17, pp. 261–269.
Wang, L. 2005. Biology of Osteogenic Sarcoma. Cancer Journal. pp. 294-305.
Ehow Health. 2011. How long are treatments for osteosarcoma. [online] Available at: http://www.ehow.com/how-does_5251031_long-treatments-osteosarcoma_.html [Accessed March 27]
Childrens Specialists. 2011. Musculoskeletal Tumors and Infections. [online] Available at: http://www.cssd.us/body.cfm?id=1238 [Accessed March 27]