Archive for January, 2011
Week 9 Year 4
Sunday, January 9th, 201109 January 2011
While on placement this week we had a patient arrive via Accident and Emergency (A&E) with a suspected abdominal obstruction. An abdominal obstruction is where there is a suspected obstruction in the small or large bowel which has become impacted. Patients being referred for suspected abdominal obstruction have to be in an upright position. The contents of the intestine and movement and motion can come to complete arrest. Symptoms usually include cramping pain, vomiting, obstinate constipation, and lack of flatus. Clinical diagnosis is confirmed through an abdominal X-ray. After carrying out the abdominal x-ray on this particular patient it was evident she had something unusual going on as the centralised part of her small bowel was extremely dilated.
Common causes of abdominal obstruction can be adhesions which usually develop after some form of pelvic surgery, hernias, and tumors. Other causes are diverticulitis, foreign bodies such as gallstones, and volvulus (twisting of bowel on its mesentery). However specific segments of the intestine are affected differently.
In a simple abdominal obstruction, a blockage can occur without any compromise to the vascular supply. All foods, fluids and digestive secretions ingested after an obstruction has occurred along with any gas accumulate above the obstruction. This causes the proximal bowel to distend, and the distal segment to collapse. This then causes the normal process of absorption and secretions of the mucosa to become depressed and congested. The bowel walls then reach deluge due to an excessive accumulation of serous fluid in the tissue spaces in the body cavity. The abdominal cavity then progresses to distend, causing strengthened peristalsis (contraction and relaxation of the alimentary canal) and an upset of the normal condition and functioning of secretions. This then increases the risks of dehydration and the advancement to a strangulating obstruction.
Strangulation of the obstructed bowel causes a compromised blood flow and can occur in a significant number of patients with small bowel obstructions. A strangulated obstruction can progress to infarction (an area of tissue death (necrosis) due to a lack of oxygen caused by obstruction) and gangrene in a short period of time.
Venous obstruction occurs first, followed by arterial occlusion (closure or blockage of a blood vessel), resulting in rapid ischemia. The ischemic bowel becomes a deluge with edema and infarcts (areas of tissue death), leading to gangrene and perforation.
Perforation can occur in an ischemic section (typically small bowel) or when there is a large amount of dilation. Perforation risk increases when the cecum is dilated to a diameter equal to or greater than 13 cm.
Symptoms and signs from an obstruction of the small bowel are usually;
• abdominal cramps around the umbilicus,
• vomiting
• partial obstruction may develop diarrhea.
• absence of strangulation, the abdomen is not tender.
• Hyperactive, high-pitched peristalsis with rushes coinciding with cramps
• dilated loops of bowel maybe palpable
• infarction, the abdomen becomes tender and auscultation reveals a silent abdomen or minimal peristalsis.
• Shock and oliguria (a low output of urine) indicate late simple obstruction or strangulation.
Symptoms and signs of a large bowel obstruction are milder symptoms. These develop gradually differing from small-bowel obstruction.
• Increasing constipation leads to obstinate constipation and distention of the abdomen
• Vomiting may occur
• Lower abdominal cramps and non-production of feces
• Examination usually shows a distended abdomen with gurgling sound caused by the movement of gas in the intestines (borborygmi).
• no tenderness, and an empty rectum
• mass corresponding to the site of an obstructing tumor may be palpable.
• Systemic symptoms are usually mild, with fluid and electrolyte deficits being uncommon.
Care for patients with small and large bowel obstruction is similar. Treatment used for an obstructed bowel can be, Nasogastric suction, IV fluids and IV antibiotics if bowel ischemia suspected. Sometimes specific measures of resection are need in adults with an obstruction of the duodenum.
If the obstruction is caused by diverticulitis a perforation is often present. If a perforation is evident then removal of the section involved is required. Resection and colostomy are then carried out, and the joining of blood vessels (anastomosis) is postponed.
Carver, E. and Carver, B. 2006. Medical imaging: techniques, reflection and evaluation. Edinburgh: Churchill Livingston Elsevier.
http://digestive.niddk.nih.gov/ddiseases/pubs/inte
http://www.merckmanuals.com/professional/sec02/ch0
Week 8 Year 4
Saturday, January 8th, 2011Week 8
This week I was out of hours. It was a quiet week; however there were a few mobile exams and a few occasions where I had to adapt my technique in order to achieve a good result. A few of these examinations being chest x-rays on patients who were unable to co-operate due to either being unconscious or medicated. I also had a few wrist x-rays pre and post manipulation where I had to adapt my technique to perform them.
Patient Positioning
The optimal positioning for obtaining a chest radiography is with the patient postero-anterior (PA) and erect (Clarks 2005). However this is not always possible, due to patient conditions some radiographs have to be obtained antero-posterior (AP) with the patient in a sitting or semi-recumbent or supine position. Patient positioning has a significant influence in the appearance of air or fluid, and blood vessels within the chest: Air usually rises to the highest point within the chest cavity. Pathologies such as a pneumothorax are mostly seen in the apex of the lung in an erect chest x-ray. When the patient is supine, the highest point in the chest lies alongside the heart and mediastinum. According to medscape 2010, a pneumothorax may cause increased lucency adjacent to these structures, which appear to have a better-defined outline than normal, often with no lung edge visible.
On an erect film any fluid lying in the lungs usually collects at the lung bases and appears as cloudy or opaque and obscures adjacent structures. Fluid levels in the lung are higher on the lateral wall of a chest image and lower at the mediastinum. When performing a supine examination, any fluid in the lungs would lie along the posterior chest wall.
A technical problem encountered by student radiographers while performing mobile chest x-rays are Lordotic AP films sometimes referred to as an apical lordotic view. A lordotic image is produced when the tube angle is not in the correct position. One of the first things you are taught when performing mobile chest exams is to always try to sit the patient as up-right as possible while giving consideration to the patients condition. Although you are taught in lectures about how a lordotic image is achieved, it sounds easy to avoid. This has been something I have had to consider a lot on placement this week.
A technique shown to me while on placement which should eliminate the chance of producing a lordotic image is to angle the tube perpendicular to the sternum so it runs parallel to the sternum and then over compensate and increase the angle down slightly more. This is now a technique which I have managed to try and has worked however I have only tried it once so I am looking forward to trying it a few times to evaluate if it works every time.
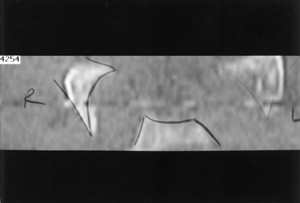
In a lordotic film the clavicles are projected higher than normal over the lung apices and the posterior and anterior ribs appear flattened. Attached to this piece of writing is a lordotic image for demonstration.
Carver, E. and Carver, B. 2006. Medical imaging: techniques, reflection and evaluation. Edinburgh: Churchill Livingston Elsevier.
Clark, K.C. 2005. Clarks positioning in radiography. 12th ed. London: Arnold.
Martensen, K.M. 2006. Radiographic image analysis. St Louis: Elservier.
http://bloggingradiography.blogspot.com/2007/07/lo
Communicating with Patients pdf
Friday, January 7th, 2011Communicating With Impaired Elderly Persons
Friday, January 7th, 2011Week 7 Year 4
Friday, January 7th, 201107 January 2011
This week I was at the Victoria hospital. Whilst there I encountered an elderly patient who was very confused and agitated. The patient was accompanied to the department by a male nurse. Before attending to her I had been told she was in an agitated state in the waiting room and had been crying and calling out to members of staff for help. On entering the room I introduced myself and explained why she was there and what she was required to do. The patient was in a wheel chair, she asked who I was and requested to see my identification badge before proceeding. Once she was satisfied that I was who I claimed to be, she continued to tell me that she had been brought in by ambulance and needed to go to the ward. I explained again that the doctor required an x-ray of her chest and he was up in the ward waiting. I took my time to explain to her we needed her to either stand or sit back in the chair for the examination, but she insisted on seeing every member of staff’s identification badge before proceeding.
It wasn’t long before we established she was not going to co-operate. We asked the male nurse if there was anyone in the ward that she recognised and trusted that could help with the patient so she would co-operate. He explained that he was new to the ward so he didn’t know. We then decided to phone the ward and ask the staff if there was anyone who could help with explaining to the patient what was required. We didn’t want to resort to sending her back without achieving the examination.
After trying everything we decided it wasn’t fair on the patient to keep pursuing the examination. It was difficult to communicate with the patient as she kept talking over the top of me when I was trying to explain why she was there and what she was there for. She demanded to see all the staffs’ identification badges that were in the room, and she would not sit up for an x-ray until she had spoken to her doctor. It was obvious no one would be able to get through to her unless she knew them or trusted them.
I found the situation a little frustrating as she seemed capable of what was required and she also seemed to understand where she was and what she needed to do but just seemed obstructive. However, if the patient is becoming agitated due to new and strange surroundings with unfamiliar faces and is also confused to what is going on, I can only imagine this will increase her fear, confusion and stress level.
Medical dictionaries define confusion as, “a state of disturbed consciousness, with disruption of thought and decision making capacity”. During my training good communication skills has always been highlighted as being essential. Having patience and a good understanding of what is required when dealing with any patient is important, however having good communication skills is vital when dealing with elderly patients especially when they are confused or frightened. According to Shank and Ratchford, confusion can be divided into two categories: acute confusion (also called delirium) and chronic confusion (also called dementia.)
Risk factors which are associated with confusion in the elderly can include normal degenerative age-related changes, as well as physical conditions, as well as emotional and social disruptions in lifestyle. Age is the best studied and the strongest risk factor for dementia. Age-related changes include the diminished ability of the brain to adapt to both internal and external changes. As aging occurs a person’s short-term memory may become less reliable than their long-term memory.
As a radiographer, it can be difficult to establish trust with elderly patients who are experiencing confusion or anxiety. We see patients for such a brief time, perform the examination and then they leave. We only have a short period of time to gain the best diagnostic images while gaining patients trust. This trust can also be difficult to maintain when having to move a patient who is in pain. However throughout my time on placement and through many experiences as an auxiliary nurse I do know how to try and gain trust from patients who are in pain or confused. By coming down to a patients eye level, and speaking slowly while having eye contact eases tension and can calm patients. I do feel if you can calm someone who is frightened it is easier to communicate with them and gain their trust. Although we were unable to gain any images for this particular patient I do feel it was the correct thing to send her back to the ward as we were only adding to her anxiety increasing her fear and confusion. I feel the nursing staff should have pre-warned us regarding the patients condition, I would do exactly the same in the future as I feel trying to force a patient or trying to achieve a diagnostic image in that type of situation could possibly have an detrimental affect. I think as a professional you should try your best to gain an x-ray, however knowing how you maybe increasing someones fear and knowing when to step back is also important.
Attached to this piece of writing are documents on communication with patient and communication with the elderly.
Lacy, K. 1998. Communicating with patients: a quick reference guide for clinicians. [online] New York: Clinical Advisory Committee. [Available at: http://www.arhp.org/uploadDocs/QRGcommunicating.pd
Communicating with impaired elderly persons. [Available at: http://www.ec-online.net/knowledge/articles/commun
Week 6 Year 4
Wednesday, January 5th, 201104 January 2011
The start of this week’s placement at Victoria hospital was fairly busy and I was able to achieve plenty of hands on experience, however by the end of the week the department was having technical problems with their equipment. I was mainly in one room for the whole of the week. On the Monday the room where I was due to be working had a problem with the table top. So we spent our time going through the appropriate examinations which were able to be performed in the room to try and keep the patients waiting time to a minimal. The work load was stream-lined to make full use of the room. By late afternoon the engineer arrived to fix the table top. Tuesday the room was up and running and the department was busy. For the next two days I really enjoyed my time in the department. I was working along side a very experienced radiographer who gave me all her attention and explained some very good techniques. One of these techniques was for a supine cervical spine examination. I have only once performed this examination and found the concept to be quite difficult to grasp, however the radiographer took the time to explain and demonstrate the procedure to allow a better understanding of the technique. Another examination she explained was in the ball catchers’ examination for rheumatology, she explained she was taught to lay the backs of the hands on the cassette and get the patient to curl their fingers slightly to look like they were going to catch something. She explained it was a necessary part of the examination was to demonstrate all joint spaces for evaluation. She explained although my technique was not wrong I could demonstrate the joint spaces better if I used her technique. I have since had the opportunity to perform the ball catchers’ examination however I have not as yet been able to perform and try the supine C-spine examination. I have previously worked with this radiographer and on every occasion she has always given me her full attention and co-operation and what I think to be valuable knowledge which I can use throughout my training.
During the week I performed an examination on a patient who was referred to the department form her General Practitioner (GP) due to onset of pain with an inability to weight bear.
I went to the waiting room and called the patient and provided her with a gown and advised her to change for the exam. Once she had changed I advised the patient I was a student in the department and asked her consent to perform the examination. While she was entering the room she seemed uncomfortable but did not complain of any pain. Once the examination was done it became obvious from the x-ray that the patient had a fracture of both the superior and inferior pubic ramus. The procedure then was to refer the patient round to the Accident and Emergency department. Fractures of the pelvis can be caused by a direct blow, e.g. direct fall, which may cause damage to the bladder or urethra, or major blood vessels.
According to Dutton (2004), the superior pubic ramus is the most commonly fractured of the pubic rami and account for more than 70% of all pelvic fractures. Signs of a pubic rami fracture are the gradual onset of pain in the groin which is aggravated by weight bearing, walking or abduction of the thigh.
According to Misra and Holmes (2004), a simple pubic rami fracture can often be discharged with analgesia following assessment of their home situation. While unstable fractures require adequate fluid resuscitation and early fixation. Most external fixation can be treated in an A&E department by experienced personnel and considerations for potential injuries, such as urethal or rectal disruption always have to be considered.
Attached to this piece of writing are images of fractured superior and inferior pubic ramus and a Medscape document on pelvic anatomy and classifications of pelvic fractures.
Dutton, M. 2004. Orthopaedic Examination, Evaluation, and Intervention. McGraw-Hill Professional Publishing, New York, New York, USA.
Misra, R. R. and Holmes, E. J. 2004. A-Z of Emergency Radiology. Cambridge University Press, West Nyack, NY, USA
http://sinoemedicalassociation.org/orthopedicsurge
http://e-radiography.net/radiology/acetabular%20fr
Week 5 Year 4
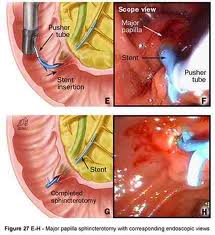
Tuesday, January 4th, 2011This week I was at Victoria Hospital. During my time this week I was assisting in Endoscopic retrograde cholangiopancreatography (ERCP). There was a full morning list and we were using a new room. I had previously screened ERCP patients in this hospital, however this was new equipment that I was being instructed on.
ERCPs are performed on patients who suffering from gallstones or experiencing problems such as jaundice. Ducts in the biliary system drain bile from the liver and pancreas. The biliary ducts and the pancreatic ducts join just before they drain into the upper bowel. This drainage opening is called the papilla and is surrounded by a circular muscle, called the sphincter of Oddi.
One patient due to have her gallstones removed had to have a biliary sphincterotomy. This is where the surgeon has to cut the muscle which surrounds the opening of the duct. This cut is made using a specialised catheter which has an electric current running through it. The surgeon was able to see stones in the gall bladder but was unable to remove them without performing the sphincterotomy. Once the sphincterotomy had been performed to enlarge the opening of the bile duct, the stones were able to be pulled from the duct into the bowel using a balloon attached to the catheter. Once the stones were removed the patient was experiencing a little bleeding. The surgeon then explained to me he was going to inject adrenaline around the site of the cut to try and minimise the bleeding. Epinephrine commonly referred to as adrenaline is a naturally produced hormone within the body, secreted by the medulla of the adrenal glands. Epinephrine, is used to contract the blood vessels around the site of the cut. Epinephrine is a hormone and a neurotransmitter. It can be used to increase the heart rate, contract blood vessels, and dilate air passages and participates in the fight or flight response of the sympathetic nervous system. Epinephrine is added to injectable forms of local anesthetics such as lidocaine as a vasoconstrictor.
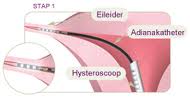
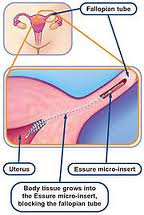
Another procedure which I performed was the screening of patients who had undergone a procedure called adiana. This procedure is a minimally invasive procedure that permanently prevents pregnancy. It works by stimulating your body’s own tissue to grow in and around tiny soft inserts that are placed inside your fallopian tubes. This is a simple procedure with a quick recovery and leaves nothing in the uterus that might limit future gynecologic procedures. It is performed by inserting a catheter into the cervix and into the uterus. This catheter delivers a low level radiofrequency (energy that generates heat to create a superficial lesion) to a small section of each fallopian tube. A tiny soft insert the size of a grain of rice is placed in each of your fallopian tubes where the radiofrequency is applied. This allows for new tissue to grow in and around the adiana inserts, eventually blocking your fallopian tubes. Patients are then sent for a hysterosalpingogram (HSG) to confirm that the tubes have been fully blocked. This test is performed to ensure that the procedure has been successful.
Attached to this piece of writing are images of both procedures.
Endoscopic Treatment for Bleeding Peptic Ulcers. 2010. Available at: http://sunzi.lib.hku.hk/hkjo/view/23/2300709.pdf [Accessed October 30 2010].
ERCP. 2010. Available at:http://emedicine.medscape.com/article/365698-imaging [Acessed October 30 2010].
Sphinterotome. 2010. Avaliable at; http://www.top5plus5.com/Procedures_files/THERAPEUTIC%20ENDOSCOPY.htm [Acessed October 30 2010].
Colonoscopy. 2011. Available at:http://www.colonoscopy-exam.info/coe/Portals/0/proc_images/procedure_images/photo14.jpg [Accessed October 30 2010].
ERCP. 2011. [online image] Avaiable at: http://www.google.co.uk/imgres?imgurl=http://www.pregnantagain.com/img [Accessed October 30 2011].
ERCP. 2011. [online image] Avaiable at:http://www.google.co.uk/imgres?imgurl=http://journals.prous.com/journals/ [Accessed October 30 2011].
Week 4 Year 3
Tuesday, January 4th, 2011SkullThis was week 4 placement and I was now at the Western General hospital. I always like working at the Western General hospital as the staff are very willing to teach and there is lots of opportunity to get of a plenty of hands on experience.
The whole week was very busy and I gained a lot of valuable experience in all aspects of the job. One examination that made me nervous was regarding a request for a patient that was due to have a Magnetic Resonance Imaging (MRI) scan. The request was to perform an orbits examination prior to him having his MRI scan due to the pre-MRI safety check, performed by the radiographer, highlighting that this patient had previously worked with metal.
I had performed an orbits exam in the past using a skull unit but was nervous about attempting it using an up-right bucky. This was due to my lack of experience in both using this equipment and being inexperienced at performing the an orbit exam. I discussed how I was going to attempt the examination with the radiographer and we agreed I would position the patient and she would check my positioning before I proceeded to complete the exam.
The basic orbits (OM) examination as stated by Carver and Carver (2006) is performed by;
• The patient seated in front of the image receptor, (this should help to ensure some stability to the patients’ posture and balance).
• The chin is placed in contact with the midline of the image receptor and the chin position adjusted until the Orbitalmeatal Baseline (OMBL) has been raised 30˚ from the horizontal plane.
• The Medial Sagital Plane (MSP) is perpendicular to the image receptor, which is assessed by checking that the External Auditory Meatus (EAMs) or lateral margins are equidistant from the image receptor.
• Centre above the External Occipital Protuberance (EOP) to emerge level with the middle of the orbits.
• Collimate to include the orbits and maxillary sinuses.
The examination was actually straight forward and once I had had time to reflect on it then it was relatively easy. The initial fear came from trying to adapt an exam that I had previously only performed using a skull unit to performing the exam on an upright bucky. On reflection, the examination was actually easier using an upright bucky than it was using the skull unit as there was less to think about in terms of positioning the cassette and the positioning angle of the skull unit.
When positioning for any examination of the skull or facial bones it is important the patient is perfectly straight with no rotation or tilt. Common errors in positioning are caused when the MSP is not parallel to the cassette and the interpupilary line is not at 90Ëš to the film. Positioning errors can be reduced by using the eyes rather than the nose as positioning aids as it is recognised that the human body is not always symmetrical.
I have very little experience in head/skull radiography and still find it intimidating and challenging especially when trying to interpret skull images. I feel from a students’ perspective it is difficult to fully understand positioning techniques from the text books. I feel observing examinations being performed and having hands on experience in all aspects of these examinations is extremely important in all types of skull examinations. However demand for plain film imaging of the head/skull has been reduced greatly due the introduction of Computed Tomography (CT) and Magnetic Resonance imaging MRI.
Attached to this piece of writing are images of a skull unit and images and diagrams of the skull taken from; http://www.e-radiography.net.
Clark, K.C. 2005. Clarks positioning in radiography. 12th ed. London: Arnold.
Week 3 Year 4
Tuesday, January 4th, 2011This was my third week at Crosshouse hospital and it was my first proper opportunity to get full time patient contact due to the previous two weeks being CT and in wards and theatres.
My skills felt quite rusty due to having no proper hands on experience for such a long period of time and I felt nervous. Protocols are also different at Crosshouse but I knew this from the last placement I had there. My first two days were mentally exhausting from double checking everything but I found it really exciting.
It was quite a slow week with not many clinics however during one orthopaedic clinic I encountered an interesting problem. The request was for a right sternoclavicular joint projection. The patient had sustained an injury which had caused subluxtion of the right sternoclavicular joint and was attending the department for a review examination from the orthopaedic consultant.
I had received a few requests from this particular orthopaedic consultant that I had not encountered before and had only read about in the positioning books which I found very interesting. These requests were for lateral scapula, sternoclavicular joints and acromioclavicular joints.
I talked the examination through with one of the radiographers; however she was also not confident in performing this exam. We then got the departments positioning book out for reference but then requested the help of a more experienced radiographer. It was acknowledged this was a rare request and due to the lack of familiarity of this particular position this examination was performed by the member of staff that felt most confident.
The positioning book dictated that we use the Kurzbauer method which states it is an unobstructed lateral projection of the sterno-clavicular articulation. This describes that the patient lies on the affected side with the arm they are lying on next to their head. Using a vertical central ray, directed 15 degrees caudally and centered to the lower most sterno-clavicular articulation. This technique was used but modified by the radiographer so the patient was positioned standing with the affected side against the upright bucky.
While observing this technique it seemed straight forward and relatively easy to perform. Once the image was obtained I found it difficult to interpret and had to get the radiographer to explain what we were looking at. After interpretation of the image it was difficult to see if any changes had occurred, as there were no previous images to compare them against. It is difficult to gain experience in these examinations since they are so rare. There was only one more request for a sternoclavicular joint that day and a different radiographer performed it while being observed.
Throughout the week I started to regain my confidence slowly with the examinations that are requested more frequently. However it took some time as I struggled to remember some protocols and also had to remember how to interact with the patients (radiology information system) RIS system.
I really enjoyed the experience of the various new referrals which had been requested while this clinic was on and I am really looking forward to tackling them in the future.
Attached to this piece of writing is an orthopaedic booklet on Sternoclavicular Joint Separation and images of the shoulder and the AC joint, and also a CT scan of a patient’s right and left sternoclavicular joints. Relative to the sternum, the left medial clavicle demonstrates 4 mm of superior subluxation. There is no detectable superior subluxation of the right medial clavicle.
Pearsall, A.W. and Russell, G.V. 2000. Ipsilateral Clavicle Fracture, Sternoclavicular Joint Subluxation, and Long Thoracic Nerve Injury: An Unusual Constellation of Injuries Sustained During Wrestling. The American Journal of sports medicine 28 (6) February, pp.904-8. Available at:http://ajs.sagepub.com/content/28/6/904.full.pdf+html [Acessed October 20 2010].
Eorthopod. 2010. Sternoclavicular problems. [online] Available at: http://www.eorthopod.com/content/sternoclavicular-joint-problems [Accessed October 20 2010].
Shoulder. 2010. Available at:http://www.projectswole.com/weight-training/the-top-5-best-shoulder-exercises/ [Accessed October 20 2010].