Week 8 Elective Placement Year 3
Tuesday, December 22nd, 2009This week I had been allocated to the rooms that deal specifically with orthopaedic clinics and walk-in GP patients. I have performed many images for the orthopaedic clinics and I feel my ability and skills have grown throughout the week.
There have been audit and review clinics all week and I have had lots of hands on experience. As well as my skills improving I feel I have established a good routine. This is something that I have been working towards for quite a while and it is good to finally have the consistency in my work that a good routine brings. I hope that I will be able to maintain this routine and carry it forward with me on my next placement.
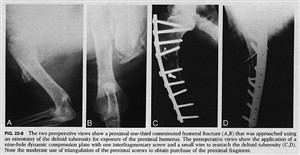
One of the more interesting experiences I have had during this placement involved a patient who had been referred to the department from an orthopaedic clinic. This patient had undergone an internal fixation to her left humerus due to a comminuted fracture 3 weeks previously but the consultant was questioning the alignment of the humerus. A comminuted fracture of a bone is where the fractured bone is in three or more pieces.
The patient was very frightened and was experiencing a large degree of pain. Due to this pain she was unwilling to move her arm. I was able to persuade her by explaining the procedure first and allowing her to manoeuvre her arm by herself; I did however advise her I would help if she needed assistance. She was understandably reluctant to remove her arm from the sling that it was in. I explained I had to take her arm out of the sling to obtain the views needed for her consultant.
To obtain the anterioposterier (AP) view I placed a set of steps with a high support handle attached to them to the left side of the patient, this allowed her to support the weight of her lower arm while she stood in position for the AP view. I explained she would be able to support her arm for the next view by placing her hand on her tummy and holding her arm away from her body. Lifting her arm from the support caused her to cry out in pain. I heard what sounded like a loose screw in the metal and a crepitus sound.
On viewing the images it was clear that 3 of the screws had dislodged from the metal work and away from the bone and the patients arm was not fixed into position. You were also able to view the segments of bone on the images which were in three separate parts. The patient was instructed to return to the orthopaedic clinic for remedial procedures.
Before leaving Perth I managed to follow up on the patient to see if she returned to theatre. The patient had been admitted to one of the wards and was scheduled to return to theatre in the next day.
Attached to this piece of writing are images of comminuted humerus fracture and fixations. The first image resembles my patient fractured humerus.